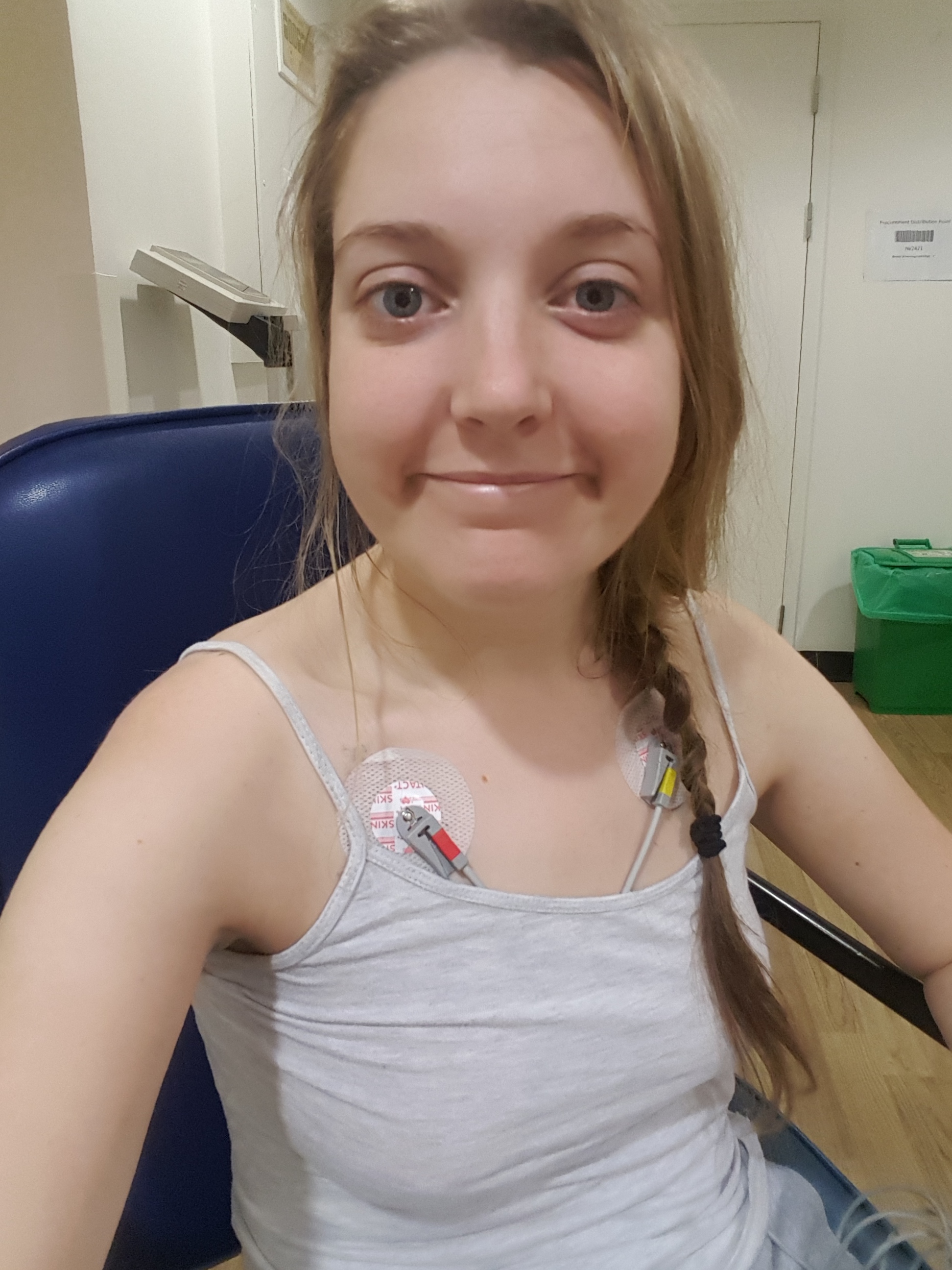
It’s what everyone’s talking about. Whether you’re out panic-buying or whether you think it’s all mass-hysteria, there’s no doubt that Coronavirus has taken over our social media feeds and is dominating our office chat. Here’s what it’s like to be amongst it all when living with active, chronic health condition.
In most cases symptoms are mild
Yes, FOR YOU. It is so frustrating to hear people in the media, offices, shops dismissing the virus, saying that symptoms are mostly mild. This may be true for the majority of people but it’s not for people like me. We know that Coronavirus can cause more severe symptoms, such as pneumonia, in people with weakened immune systems, older people, and those with long-term health conditions. Pneumonia is no joke – certainly not in addition to Lupus. So, for you, Coronavirus might simply be the risk of mild flu-like illness, but for me, it’s a whole lot more than that.
More people die of flu
Yes, we know, because we spend all winter trying to avoid getting that too. Catching flu is also a huge risk to those of us living with chronic health conditions. There are key differences with Coronavirus though. We are vaccinated at the end of summer to protect us against seasonal flu. We are also protected to some extent by the fact that a lot of the population has immunity against seasonal flu. Currently, no one has immunity to Coronavirus which means it spreads much more rapidly through the population, making it more likely to spread to us. Evidence suggests that Covid-19 is also more contagious than seasonal flu, with its infection rate around twice as high as that for seasonal flu. Comparing Coronavirus to seasonal flu is not entirely helpful though. The symptoms of Coronavirus are more severe than flu, and with that, more deadly. The death rate for seasonal flu is around 0.1 per cent while Covid-19 proves deadly in around 3.5 per cent of confirmed cases. Serious cases can also occur in relatively young people with no prior health conditions.
Stockpiling is frowned upon
For people with chronic illness, stockpiling is a part of normal life. Supermarkets are a hotbed of infection for we immuno-compromised so every trip to one is carefully planned. We don’t have the luxury of dropping into Tesco after work to see what we fancy for dinner because every time we touch a trolley or basket, or are stood in front of the incessant sneezer in the queue, we put ourselves at risk. We have to keep our cupboards stocked of essential items and our freezers full of back-up meals because sometimes we don’t have the energy to get out of bed. I’m not talking about that ‘oh I can’t be bothered to cook tonight’ feeling, I mean the crushing fatigue that makes walking to the bathroom feel like wading through quicksand.
Family and friends
Many people with health conditions, and other vulnerable people, rely on family and friends for support with daily life. And many of us don’t live in an environment where we can self-isolate from those we live with. That makes Coronavirus also really scary for those who have loved ones living with chronic health conditions. While they may be able to withstand the ‘mild symptoms’, the thought of bringing it home to a vulnerable loved-one is terrifying.
Seeing the invisible
Coronavirus is giving many people an insight into the world of those living with disability or illness. The people who are forced into self-isolation due to the risk of infection or ill-health. The people who have had to leave careers due to the lack of flexibility or understanding from employers or colleagues. And they did so with no one watching. It’s great that measures are being introduced to support people in remote working and financially during the Coronavirus crisis but we should not forget that there are many people in our society for whom this has become ‘normal life’. They were isolated before there were articles on how to cope with the anxiety of isolation or how to work from home effectively.
The Coronavirus has demonstrated that people who are isolated need not be invisible. Yet, there is a whole community of people with disability or chronic illness for whom isolation is a reality, with or without the threat of Covid-19. If there’s one good thing that comes out of this, it should be a commitment to them. We should empower this community to participate in our society. Because we have so much to learn from their strength and resilience in the face of adversity, and they deserve to be seen.
What can you do?
Try not to dismiss people’s concerns about Coronavirus. They might be living with a health condition, or they might live with or care for someone who does. Regardless of how you interpret your personal risk, we know that people with health conditions are at high risk of developing complications which can be life-threatening. Try not to judge people who you deem to be stockpiling. They may be doing their once-fortnightly shop or they might be buying items for vulnerable family or friends. Follow the Government advice, but understand that some people need to go further than this. Take responsibility for your role in slowing the spread of the virus, as well as other viruses and colds. With remote working accessible for many people, there’s really no need to be a martyr. Anyone with Lupus or another chronic illness will tell you that your good health is the greatest gift of all so protect it with all you’ve got. And connect with those who are isolated and vulnerable. When we unite as a community to support and carry each other, there’s nothing we can’t get through. After all, in the words of the late Ram Dass, “we’re all just walking each other home.”