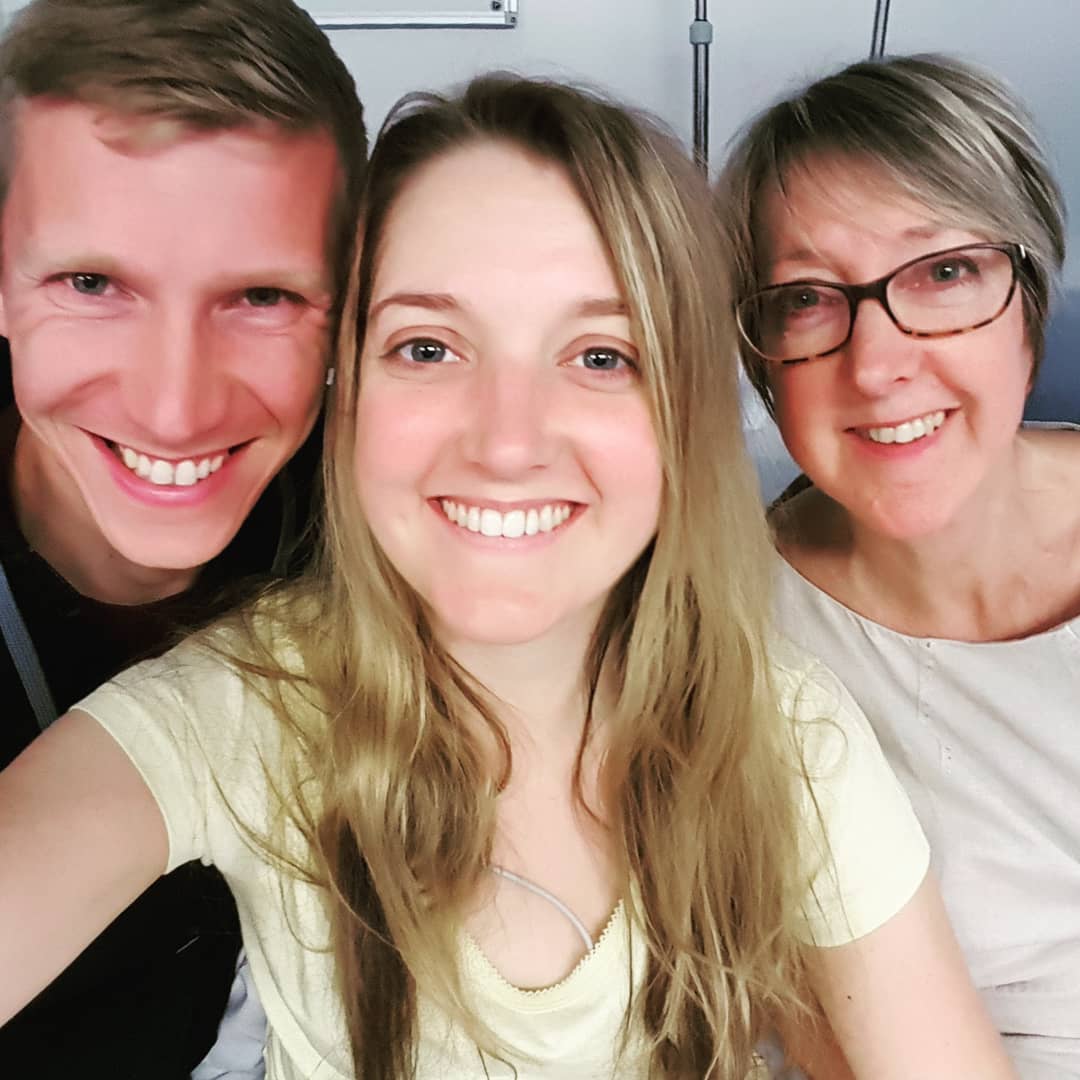
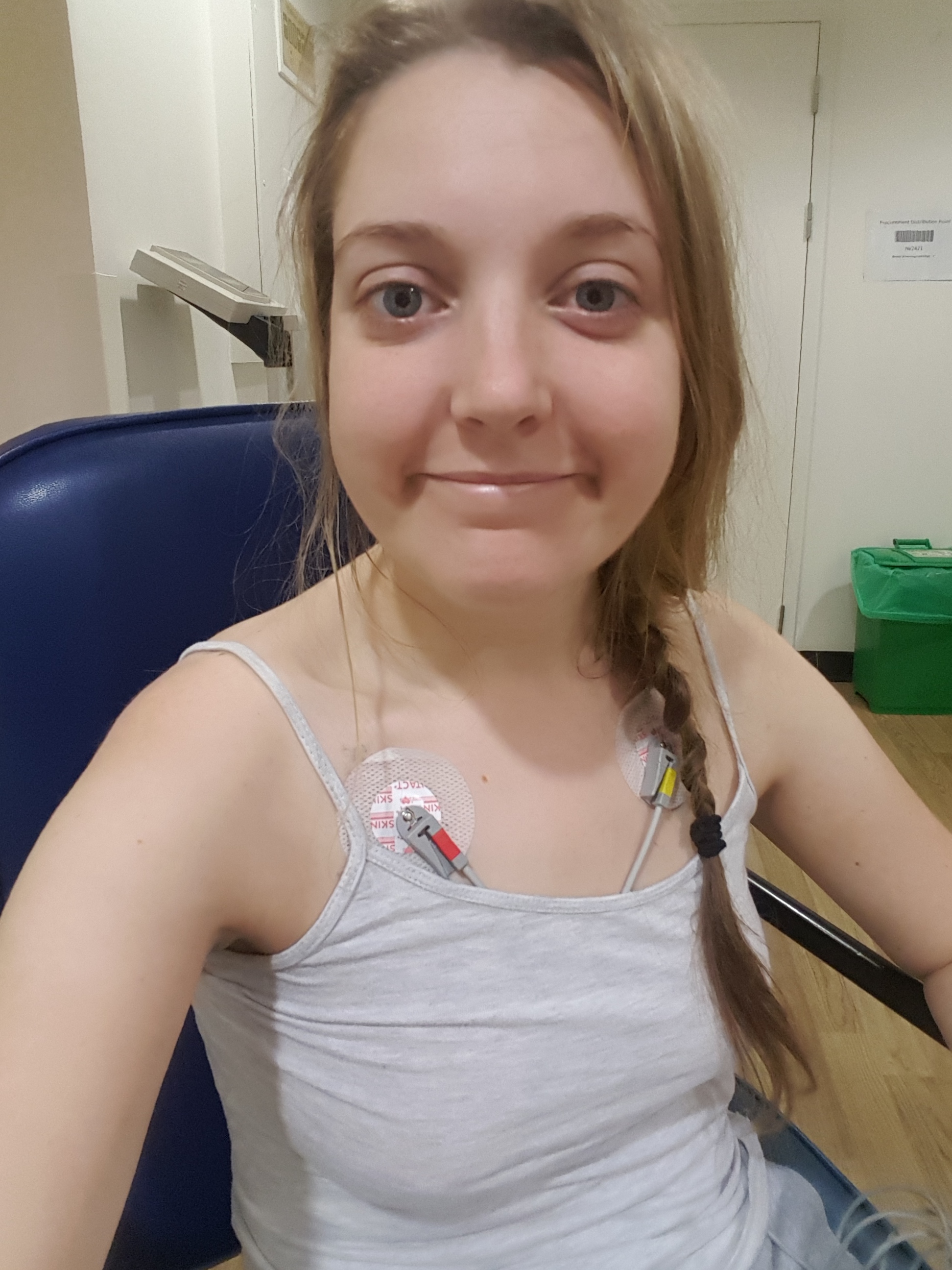
So, I’m losing my hair. That’s right, on top of everything else that’s going on in my body, my hair is falling out. Just what you want 3 months before your wedding! After a couple of weeks of denial, this is my call to arms. I’m calling all of you who have ever suffered thinning, brittle hair or hair loss and you general hair gurus for all your hints and tips to see if we can save my mane!
Why hair loss?
Apparently hair loss is quite common in Lupus. It can be a symptom of the Lupus itself or a side effect of treatment. Although in some cases scarring can cause lasting damage to the follicles, in most cases it grows back in time when the active disease is under control. Hair loss caused by medication (which I think mine mostly is) tends to be reversible. But we are on a 3 month deadline! Brittle hair is caused by steroids, and immunosuppressants cause thinning. Oh, and stressing about your hair loss also causes hair loss.
You’d think we Lupus sufferers have enough to deal with what with the organ failure, joint pain, muscle pain, inflammation, chronic fatigue, skin rashes, the list goes on… BUT I realised today that instead of feeling sorry for myself or distressed at this horrible Lupus side effect, maybe this is one I can seize control of and do something to prevent or slow down? So, this is my call to arms! Below are some questions I have – let me know if you have any hints or tips for me to try. I’ll let you know how I get on.
- When should I brush my hair? My hair is VERY brittle and dry but also extremely knotty. Should I brush it wet, dry, first thing in the morning, last thing at night, often or not at all? What kind of brush should I use?
- Should I cut it? I haven’t had it cut since January so it does need a trim. Should I just cut the split ends off or should I have a good length off? Ideally I want to preserve some length for the wedding but does cutting it encourage growth? How many times should I look to have it cut between now and the wedding? Could you, or a hairdresser you know, come to my house to cut it for me? I’m not able to leave the house really but it probably needs doing before my hair trial on 27 July!
- What about colour? I usually have half a head of highlights twice a year. I was planning on having it done in the summer and then a few weeks before the wedding in October but should I hold fire if it could damage my hair? Ideally I’d have it just before my hen do in August and then again before the wedding for that fresh look but I’m worried about damaging my hair further.
- What products should I use? At the moment I use Aussie shampoo and conditioner and wash it every 3 – 4 days. Should I use a deep moisture treatment and if so, which one? Are there any other products I could use? Or maybe I shouldn’t use products at all?
- How often should I wash it? Should I try to wash it more frequently or less often than every 3 – 4 days? Is there a certain way I should try to wash my hair? At the moment I am steering clear of blow drying and straightening, is this the right thing?
- How to cover thinning? I’m mostly thinning around my hair line – any tips for covering this? Is there something I can do with accessories or make up to try to help?
- A back up plan? What should my back up plan be for the hen do & wedding? Should I be thinking wig, hair extentions, crown volumiser? Where do I start?
Comment below or contact me on facebook or Instagram Livin’LaVidaLupus for any advice you have!